What is a portosystemic shunt?
Blood from the gastrointestinal tract, spleen and pancreas drains through a network of veins into a larger vein called the portal vein, which in turn flows through the liver. This blood contains the breakdown products of digestion which, if released into the general circulation, would be toxic to the body. The liver, therefore, filters these products and turns them into less harmful and more useful substances prior to their entering the general circulation of the rest of the body.
A portosystemic shunt is a blood vessel which connects the portal vein (or one of its tributaries) to the systemic circulation (usually the vena cava), thus bypassing the liver. This means that the body is exposed to potentially harmful protein breakdown products.
In cats and dogs, portosystemic shunts are almost always congenital. Portosystemic shunts may be extrahepatic (outside the liver) or intrahepatic (inside the liver). As a rule, small to medium dogs and cats have extrahepatic shunts, whereas larger dogs have intrahepatic shunts, though there are exceptions to this generalisation. Extrahepatic shunts are usually readily accessible by surgery. Intrahepatic shunts are sometimes accessible and sometimes not, and operating on these shunts is technically more demanding and riskier for the patient.
Intrahepatic shunt
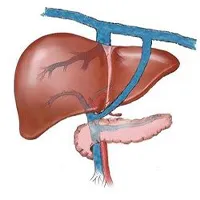
Extrahepatic shunt
What clinical signs might my pet show if it has a portosystemic shunt?
Portal blood flow to the liver is important to allow normal liver growth and function. In turn, the liver has an important role in forming the building blocks for other body systems and allowing normal growth. Patients with a portosystemic shunt have impaired liver function and are often small compared with their littermates and underweight.
When portal blood bypasses the liver, the body is exposed to potentially harmful protein breakdown products, and these can affect different areas of the body:
- Central nervous system. Certain protein breakdown products, particularly ammonia, can cross the blood-brain barrier and exert toxic effects on the brain. This can result in a myriad of neurological abnormalities such as altered behaviour, depression, disorientation, central blindness, tremors, seizures and coma. Hypersalivation is very commonly seen in cats. The neurological manifestations of portosystemic shunting are collectively referred to as hepatic encephalopathy (HE).
- Gastrointestinal system. Abnormal gastrointestinal function is common resulting in poor appetite, vomiting and diarrhoea. Affected patients often fail to thrive. Some dogs exhibit pica, whereby they regularly eat items not considered to be edible such as stones.
- Urinary system. Patients with portosystemic shunts have impaired hepatic metabolism of ammonia and uric acid. These products are excreted in the urine where they can form bladder stones. This can result in cystitis, and in male dogs there is a risk that stones can pass out of the bladder into the urethra, resulting in acute and life-threatening urinary obstruction.
How are portosystemic shunts diagnosed?
There is a large variation in the type and severity of presenting signs in patients with a portosystemic shunt, and your vet will often run a number of blood tests in order to reach a diagnosis.
Non-specific findings in patients with portosystemic shunts include anaemia, low albumin, low urea and low cholesterol.
Your vet will also recommend specific tests to look at liver function, typically dynamic bile acids and ammonia. Bile acids are released by the gallbladder to aid digestion and then reabsorbed via the portal system by the liver. This process fails in patients with a portosystemic shunt and bile acids tend to be very high in fasted patients and especially in patients that have recently been fed. Ammonia is a protein waste product that should be metabolised by the liver. It is often markedly elevated in patients with a portosystemic shunt.
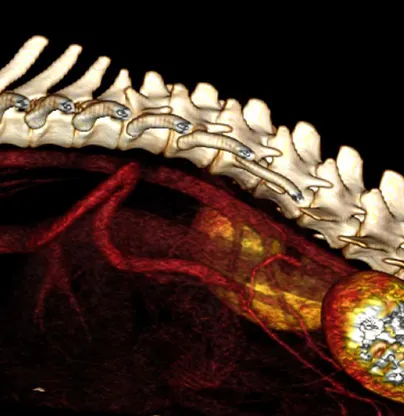
To definitively diagnose a portosystemic shunt, advanced imaging is required. At Swift, we perform CT-angiography, which is the gold-standard method of diagnosing portosystemic shunts. This safe and non-invasive test involves obtaining a CT scan of your pet after a dye is given into the bloodstream. This lights up the shunt and surrounding vasculature, confirming the diagnosis. It also provides very important information about the location and anatomy of the shunt, which is essential for surgical planning.
How are portosystemic shunts treated?
Portosystemic shunts can be treated medically or surgically. Medical treatment is almost always recommended for a few weeks prior to surgery in order to make these patients safer anaesthetic and surgical candidates. While medical management can help to control some of the symptoms of portosystemic shunting, it is widely considered that surgical management provides better long-term control and quality of life. Medical management typically comprises:
- Diet. Traditionally diets with restricted protein and highly digestible carbohydrates were recommended in these patients to reduce the number of harmful breakdown products such as ammonia and certain amino acids. Younger, growing patients with portosystemic shunts may not be able to cope with severe protein restriction, and in these patients your vet may recommend an alternative protein source such as soya.
- Lactulose. This is a disaccharide laxative that traps ammonia in the colon, thus limiting its absorption and its adverse effects on the central nervous system.
- Antibiotics. Antibiotics are recommended to reduce the load of ammonia-producing bacteria in the gut. It is unclear in veterinary patients how much benefit there is to antibiotic use over and above diet and lactulose, and their use may be better limited to more severely affected patients. When used, ampicillin or metronidazole are the antibiotics of choice.
- Anti-seizure medication. There is some evidence to suggest that using anti-seizure medication (usually levetiracetam) prior to surgery may decrease the incidence of seizures after surgery. The evidence for this is weak and the use of such drugs is often reserved for patients who have seizures prior to surgery owing to their hepatic encephalopathy rather than for general use in all patients.
Surgical Treatment of Portosystemic Shunts.
The goal of surgical treatment is to achieve closure of the portosystemic shunt, thus redirecting portal blood flow through the liver and restoring normal liver function. Surgery entails a standard approach to the abdominal cavity called a celiotomy. Extrahepatic shunts are readily identifiable and accessible by surgery. Only around 15% of shunts can be fully ligated at the time of surgery. This is because in many patients the portal system within the liver is underdeveloped and is unable to cope with a sudden increase in blood flow. If this were to happen, a life-threatening condition called acute portal hypertension could arise. Therefore it is considered safer to apply a device around the shunt which will gradually occlude it over a few weeks, allowing time for the liver’s portal system to develop and accommodate the increased blood flow. The most commonly used devices are ameroid constrictors or cellophane bands.
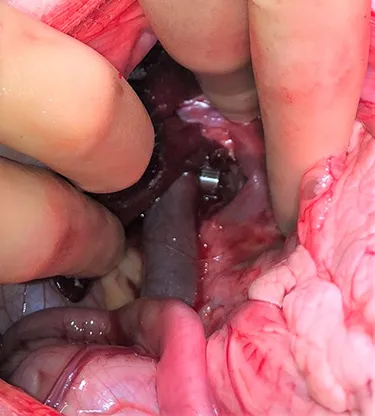
Intrahepatic shunts can also be treated surgically, though these are technically more difficult to access and the risks during surgery are greater. Intrahepatic shunts are also treated by a minimally invasive procedure called transvenous coil embolization.
What are the outcomes following surgery?
All surgical procedures carry a risk and we can see the following complications in some patients:
- Acute portal hypertension. If the shunt closes prematurely the liver is not usually able to cope with the increased blood flow and we can see pressure elevations in the portal blood vessels. This can cause abdominal pain, damage to the gastrointestinal tract, a build up of fluid in the abdominal cavity and death. Thankfully, with the use of devices that gradually close the shunt, this phenomenon is rarely if ever seen.
- Incomplete closure of the shunt. The main drawback of devices that allow gradual shunt closure is that they do not always achieve complete closure of the shunt, which means that a fraction of portal blood will continue to bypass the liver. In the majority of patients this doesn’t cause any clinical signs, but some patients may require long-term medication or a second surgery to fully close the shunt.
- Multiple acquired shunts. In some patients the liver is never able to accommodate increased portal blood flow following shunt closure, and the body’s response is to open up new shunts to allow this blood to continue to bypass the liver. If this arises, lifelong medication is necessary.
- Post-attenuation neurological signs. Some patients can develop neurological abnormalities such as seizures after shunt surgery. These signs can be mild and transient or more severe and longstanding. The cause of this is unknown and treatment can be difficult. It is difficult to predict which patients will develop this problem but the risks do seem to be higher in patients that had serious neurological dysfunction prior to surgery.
In spite of these risks, patients undergoing surgery to attenuate extrahepatic portosystemic shunts usually have a good to excellent outcome, with very low peri-operative mortality rates and with most patients being able to live normal lives without symptoms or medication. The risks during surgery are greater for patients who have intrahepatic shunts. Nevertheless, many patients still enjoy good long-term outcomes following surgery.
Portosystemic shunt surgery is usually only performed by specialist surgeons who have extensive experience performing this type of surgery, as is the case at Swift Referrals.